Managing blood sugar is one of the most important steps you can take for long-term health. When your blood sugar stays too high for long periods, it puts stress on your body. High blood sugar, also called hyperglycemia, increases your risk of type 2 diabetes, heart disease, stroke, nerve damage, and even vision problems. Over time, these conditions can lower your quality of life and make daily activities more difficult.
This is why many people look for natural and simple ways to keep their blood sugar in balance. One approach that has gained a lot of attention is intermittent fasting (IF). Instead of focusing on strict diets or cutting out certain foods, intermittent fasting changes when you eat. Many studies suggest this pattern can help reduce blood sugar spikes, improve insulin sensitivity, and support weight loss—all of which play a role in better glucose control.
But how does intermittent fasting really affect your blood sugar? Can it work for people with diabetes, or is it only safe for healthy individuals? And what does the latest science say about fasting and blood sugar? Let’s break it down in simple terms so you can decide if it’s right for you.
What Is Intermittent Fasting?
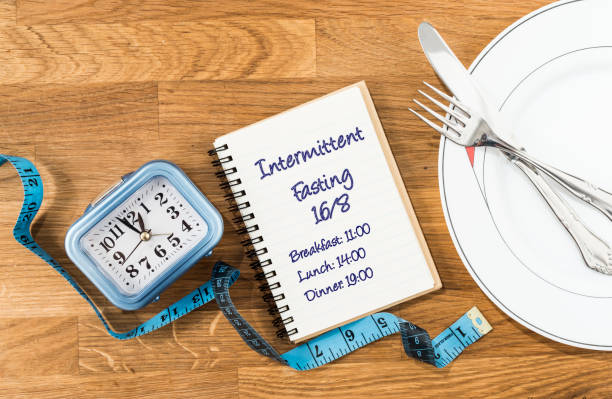
Intermittent fasting is not a diet—it’s an eating pattern. Instead of focusing on what you eat, it focuses on when you eat. This makes it different from most diets, which often restrict calories or cut out entire food groups. With intermittent fasting, the timing of your meals matters most, and your body spends part of the day in a fasting state.
Some common methods include:
- 16/8 method: Fast for 16 hours, eat within an 8-hour window. This is the most popular style because it fits easily into most lifestyles. For example, you might eat from 12 p.m. to 8 p.m. and fast the rest of the time.
- 5:2 method: Eat normally 5 days a week, and eat only 500–600 calories on 2 non-consecutive days. This approach helps cut calories while still giving you flexibility during the week.
- Alternate-day fasting: Fast every other day, either eating very little or nothing at all on fasting days. This is more challenging but may bring quicker results for some people.
During the fasting window, you usually drink only water, black coffee, or unsweetened tea. These drinks don’t raise blood sugar or break your fast, which makes them safe to consume while fasting. Some people also include sparkling water or herbal teas to help reduce hunger.
By cycling between eating and fasting, your body has more time to use stored glucose, improve insulin sensitivity, and even burn fat for energy. This shift in fuel use is one of the main reasons intermittent fasting may help with blood sugar control.

How Intermittent Fasting Affects Blood Sugar
One of the biggest reasons people try intermittent fasting is to stabilize their blood sugar. Here’s what happens in your body:
1. Reduced Blood Sugar Spikes
When you fast, your body has more time to process glucose (sugar from food) and bring levels back to normal. Without constant eating, your digestive system gets a break, and your insulin levels have time to drop. This helps your cells become more sensitive to insulin, so they can absorb sugar from the blood more effectively.
Studies show that intermittent fasting can reduce blood sugar spikes after meals and improve overall glucose levels throughout the day. This means fewer sharp rises and crashes, which often lead to fatigue, cravings, and weight gain. Over time, keeping blood sugar steady may also lower the risk of insulin resistance, prediabetes, and type 2 diabetes.
For many people, this makes intermittent fasting a powerful tool for blood sugar management, especially when combined with a balanced diet and regular exercise.
👉 According to the American Diabetes Association, controlling post-meal blood sugar is key to preventing long-term complications.
2. Improved Insulin Sensitivity
Insulin is the hormone that helps your cells absorb glucose and use it for energy. After you eat, your blood sugar rises, and insulin acts like a key, unlocking your cells so glucose can enter. But when your body stops responding to insulin well, sugar stays in the bloodstream instead of moving into your cells. This condition is called insulin resistance, and it is one of the main risk factors for type 2 diabetes.
Over time, insulin resistance forces the body to produce more and more insulin, which can strain the pancreas and make blood sugar harder to control. This is where intermittent fasting may help. Research shows that intermittent fasting can improve insulin sensitivity, meaning your cells respond better to insulin and absorb glucose more effectively.
Better insulin sensitivity not only lowers blood sugar but also reduces the risk of weight gain, inflammation, and other problems linked to metabolic syndrome. This is one of the main reasons experts believe intermittent fasting is a useful tool for supporting long-term blood sugar control.
3. Lower Risk of Type 2 Diabetes
A review published in the journal Nutrients found that intermittent fasting can help reduce fasting glucose levels and may lower the risk of developing type 2 diabetes. Fasting glucose is the measure of blood sugar after you have not eaten for several hours, usually overnight. High fasting glucose is often an early warning sign of prediabetes, which can progress to type 2 diabetes if not managed.
By lowering fasting glucose, intermittent fasting helps the body maintain more stable blood sugar throughout the day. The review also noted that fasting may improve other markers linked to diabetes risk, such as insulin resistance, body weight, and inflammation. Together, these changes can make it easier for the body to control glucose and reduce stress on the pancreas.
While more long-term studies are needed, current evidence suggests that intermittent fasting could be an effective lifestyle strategy for people who want to prevent or delay type 2 diabetes naturally.
Intermittent Fasting for People with Diabetes
If you have diabetes, you may wonder if intermittent fasting is safe. The answer: it depends.
- Type 2 diabetes: IF may help reduce insulin resistance and promote weight loss, both of which improve blood sugar control.
- Type 1 diabetes: IF can be risky since it increases the chance of hypoglycemia (low blood sugar). Always talk to your doctor first.
⚠️ Important: If you’re on blood sugar–lowering medications like insulin or sulfonylureas, fasting may cause dangerous drops in glucose. Never start intermittent fasting without medical supervision.
For more safety information, check out Harvard Health Publishing.

Benefits of Intermittent Fasting Beyond Blood Sugar
Intermittent fasting isn’t just about glucose control. Many people experience other health benefits, such as:
- Weight loss – Eating in shorter windows often reduces calorie intake naturally.
- Reduced inflammation – Fasting gives your body time to repair and may reduce chronic inflammation.
- Heart health – Studies suggest IF may improve cholesterol and blood pressure.
- Cell repair – Fasting activates autophagy, a process where cells clean out damaged parts.
These benefits all play a role in better metabolic health, which further supports stable blood sugar.
Potential Risks and Side Effects
Like any lifestyle change, intermittent fasting comes with potential risks. Common side effects include:
- Hunger and irritability
- Headaches or dizziness
- Low energy during fasting periods
- Risk of binge eating during eating windows
People who should avoid intermittent fasting include:
- Pregnant or breastfeeding women
- Children and teenagers
- People with a history of eating disorders
- Anyone with chronic health conditions without doctor approval
How to Start Intermittent Fasting Safely for Blood Sugar
If you want to try intermittent fasting to support healthy blood sugar, here are some practical tips:
1. Start Slowly
Don’t jump straight into long fasts. Begin with a 12/12 method—12 hours of fasting, 12 hours of eating—and gradually increase your fasting window.
2. Stay Hydrated
Drink water, herbal tea, or black coffee during fasting hours to avoid dehydration.
3. Eat Balanced Meals
When you break your fast, focus on:
- Lean proteins (chicken, fish, eggs)
- Fiber-rich carbs (vegetables, beans, whole grains)
- Healthy fats (avocado, olive oil, nuts)
This helps keep your blood sugar stable.
4. Monitor Your Blood Sugar
If you have diabetes, check your glucose regularly, especially in the first few weeks.
5. Combine with Exercise
Light exercise such as walking, yoga, or resistance training can further improve insulin sensitivity.
Intermittent Fasting vs. Other Diet Approaches for Blood Sugar
How does intermittent fasting compare to other popular eating styles?
- Low-carb diet: Focuses on reducing carbs to limit blood sugar spikes.
- Mediterranean diet: Emphasizes whole foods, fish, olive oil, and vegetables.
- Plant-based diet: High in fiber, which slows glucose absorption.
The key difference is that intermittent fasting is about timing, while other diets are about food choices. Many people combine IF with a healthy eating plan for the best results.

Frequently Asked Questions About Intermittent Fasting and Blood Sugar
Does intermittent fasting cause low blood sugar?
For most healthy people, no. But if you take diabetes medications, fasting can lower your glucose too much.
How long before I see results?
Many people notice improved energy and lower fasting glucose in 2–4 weeks.
Can I drink coffee while fasting?
Yes, as long as it’s black and unsweetened.
Is intermittent fasting safe long term?
Studies suggest it can be safe for many people, but more research is needed. Always listen to your body.
Key Takeaways
- Intermittent fasting can improve blood sugar by lowering glucose levels and boosting insulin sensitivity.
- It may reduce the risk of type 2 diabetes when combined with a healthy lifestyle.
- IF is not safe for everyone, especially those with type 1 diabetes, certain medical conditions, or on specific medications.
- Starting slowly, staying hydrated, and eating balanced meals are crucial for success.
Conclusion: Should You Try Intermittent Fasting for Blood Sugar?
Intermittent fasting shows great promise for managing blood sugar and improving overall health. While it isn’t a one-size-fits-all solution, research suggests it can be a powerful tool when used safely and consistently.
If you’re curious, start small and track how your body responds. And if you have diabetes or any medical condition, talk with your doctor before trying it.
💬 Now it’s your turn!
Have you tried intermittent fasting to manage blood sugar? What worked—or didn’t—for you? Share your experience in the comments below!