Why Your Gut Health Matters If You Care About Blood Sugar
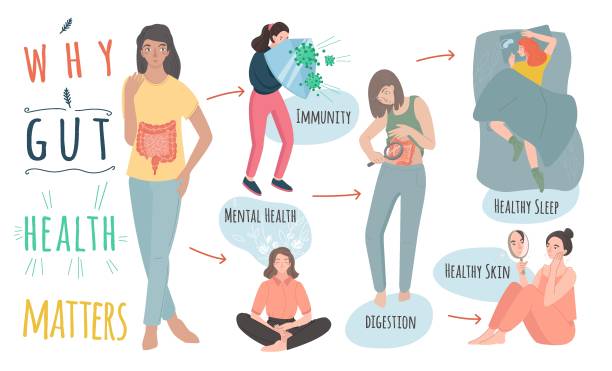
Your gut is home to trillions of tiny microbes—bacteria, fungi, and other microorganisms that form what’s known as the gut microbiome. These microbes do much more than just help digest food. They produce essential vitamins like B12 and K, support your immune system, and even send chemical signals that affect your mood and metabolism. When your gut bacteria are balanced and diverse, your body runs more smoothly—you absorb nutrients better, reduce inflammation, and maintain steady blood sugar levels.
But when that balance is disrupted—a condition called gut dysbiosis—trouble begins. Harmful bacteria can multiply, triggering inflammation and damaging the gut lining. This “leaky gut” allows toxins to enter the bloodstream, which can confuse your immune system and interfere with insulin signaling. Over time, this can make your cells resistant to insulin, a major step toward type 2 diabetes.
In fact, research over the past decade has revealed a strong connection between the gut microbiome and metabolic health. Studies published in scientific journals like PubMed Central (PMC) show that people with type 2 diabetes often have lower levels of beneficial bacteria such as Akkermansia muciniphila and Bifidobacterium, along with higher levels of inflammation-causing microbes. Supporting a healthy gut—through diet, probiotics, and lifestyle choices—may therefore play a key role in preventing or managing diabetes naturally.
What Is the Gut Microbiome?
The gut microbiome is the community of bacteria, yeasts, and other tiny organisms in your digestive tract. Most live in your large intestine. A healthy, diverse mix of these microbes helps break down fiber, turn it into helpful compounds, and protect your gut lining. Lower diversity and “dysbiosis” (an unhealthy balance) are often seen in people with prediabetes and type 2 diabetes. (PMC)
How Gut Health Connects to Diabetes
1) Short-Chain Fatty Acids (SCFAs) and Insulin Sensitivity
When you eat fiber, gut bacteria make short-chain fatty acids like acetate, propionate, and butyrate. These support a strong gut lining, reduce inflammation, and may improve insulin sensitivity. Lower SCFA levels are linked with obesity and type 2 diabetes. Some clinical studies show SCFA-raising strategies can help fasting glucose and insulin, though results vary. (PMC, PubMed)
Bottom line: more fiber → more SCFAs → better gut and metabolic health.
2) Gut Barrier and Inflammation
A healthy gut barrier keeps unwanted molecules out of your bloodstream. When that barrier weakens, it can trigger immune stress and low-grade inflammation. That inflammation can worsen insulin resistance. Restoring a healthy microbial balance may help calm that process. (PMC)
3) Hormones From the Gut (like GLP-1)
Your gut talks to your pancreas and brain using hormones such as GLP-1, which helps control appetite and blood sugar. New research suggests some diabetes and weight-loss drugs (GLP-1 receptor agonists) may also shift the microbiome. We are still learning how much of their benefit comes through gut changes, but the link is promising. (PMC)
4) Bile Acids and Metabolism
Gut microbes help convert bile acids into forms that can affect blood sugar and energy burn. Changes in these pathways may play a role in insulin resistance. (PMC)

Medications and the Microbiome: What We Know
Metformin, a first-line type 2 diabetes drug, does more than lower glucose. Studies show it can change the gut microbiome—often increasing beneficial species like Akkermansia and bacteria that make SCFAs. These shifts may be part of metformin’s glucose-lowering effect. (PMC, Frontiers, ScienceDirect)
GLP-1 medicines (like liraglutide and semaglutide) may also influence gut microbes, though human data are still limited for some drugs. This is an active area of research. (PMC)
Important: Never change or stop medications without talking to your healthcare provider.
The Evidence in Plain English
- People with prediabetes and type 2 diabetes often show lower gut microbial diversity and different species patterns. (PMC)
- Fiber-rich diets support SCFA-producing bacteria, which can help with blood sugar control. (The Nutrition Source, Harvard Health)
- Fermented foods can increase microbiome diversity and may lower inflammatory markers. (Stanford Medicine, Cell)
- The microbiome may even play a causal role in certain diabetes subtypes, though this is still being tested. (PMC)
Prebiotics, Probiotics, and Postbiotics—What’s the Difference?
- Prebiotics are substrates “selectively utilized by host microorganisms, conferring a health benefit.” Many are types of soluble fiber found in plants. Think inulin, FOS, GOS, and resistant starch. (isappscience.org)
- Probiotics are “live microorganisms that, when given in adequate amounts, confer a health benefit.” Not all fermented foods or yogurts meet this standard, but many do. Check labels for strain and CFU info. (isappscience.org)
- Postbiotics are inactivated microbes or their components that still offer a benefit. This is a newer category with growing research. (Nature, isappscience.org)

What to Eat for a Gut-Friendly, Glucose-Friendly Plate
1) Load Up on Fiber (Daily)
Aim to fill half your plate with vegetables and add legumes, whole grains, nuts, and seeds. Soluble fiber forms a gel that slows digestion and helps prevent glucose spikes. It also feeds SCFA-producing microbes. (The Nutrition Source, CDC)
High-fiber picks:
- Beans, lentils, chickpeas
- Oats, barley, quinoa, brown rice
- Chia, flax, walnuts, almonds
- Apples, berries, citrus
- Broccoli, Brussels sprouts, leafy greens
2) Include Fermented Foods (Most Days)
Yogurt with live cultures, kefir, kimchi, sauerkraut, miso, tempeh, and certain aged cheeses can boost microbiome diversity. Start small if you’re new to them. (Stanford Medicine, PMC)
3) Choose Smart Carbs and Cooking Methods
Whole, minimally processed carbs plus fiber and protein keep blood sugar steadier. Even how you cook starchy foods matters. For example, regularly eating deep-fried potatoes (like fries) is linked with a higher risk of type 2 diabetes, while baked or boiled potatoes do not show the same risk pattern. Replacing fries with whole grains can lower risk. (Harvard Chan School of Public Health)
4) Add Resistant Starch
Cooling cooked potatoes, rice, or pasta in the fridge and eating them later (or reheated) can increase resistant starch, which acts like prebiotic fiber. (General nutrition concept; individual responses vary.)
5) Mind Your Fats
Olive oil, nuts, and fatty fish fit well in a gut-friendly, diabetes-aware diet. They help with satiety and can support healthier lipid profiles.
6) Hydrate and Move
Water helps fiber do its job. Light movement after meals—like a 10–15 minute walk—can also support blood sugar control.
Simple 1-Day Gut-and-Glucose Sample Menu
Breakfast
- Overnight oats with chia, plain yogurt or kefir, berries, and walnuts
- Green tea or water
Lunch
- Lentil and veggie bowl with olive oil, lemon, and herbs
- Side of sauerkraut or kimchi
- Sparkling water
Snack
- Apple slices with peanut butter
- A few almonds
Dinner
- Grilled salmon or tofu
- Quinoa or cooled-and-reheated brown rice (for resistant starch)
- Roasted broccoli and carrots
- Small side salad with olive oil and vinegar
Dessert (optional)
- A square of dark chocolate (mind portions)
- Herbal tea
Do You Need a Probiotic Supplement?
Food first is a great rule. If you choose a supplement, look for:
- Documented strain(s) and CFU amount through shelf life
- Evidence for the benefit you want (e.g., antibiotic-associated diarrhea)
- Quality testing and clear labels
Use probiotics with care if you have a weakened immune system or other medical issues. When in doubt, talk to your healthcare team. (ISAPP has helpful consumer guides on what probiotics are and how to read labels.) (isappscience.org)
Lifestyle Habits That Support Gut and Metabolic Health
- Follow a fiber-rich eating pattern. It helps with weight, satiety, and blood sugar. (Harvard Health)
- Stay active. Aim for regular movement you enjoy.
- Sleep well and manage stress. Both influence hunger, choices, and insulin sensitivity.
- Do not smoke. Smoking harms gut health and raises diabetes risk.
- Join a proven lifestyle program if you’re at risk. CDC-recognized programs can cut type 2 diabetes risk by about half for many people. (CDC Stacks)
FAQs
Is there proof that changing my gut can change my blood sugar?
Growing research links gut patterns to blood sugar control and diabetes risk. Some trials show that adding fiber and fermented foods can improve markers linked to inflammation and insulin resistance. Not every study shows the same result, but the trend is positive and the habits are low-risk and healthy. (Stanford Medicine, PubMed)
Can certain drugs “fix” the microbiome?
Metformin likely helps shift the microbiome toward a healthier balance and may raise SCFA producers. GLP-1 drugs also appear to affect gut microbes, but human data are still emerging. These drugs work through multiple pathways; the microbiome is one part of the story. (PMC, Frontiers)
Should I avoid potatoes?
Not necessarily. Preparation is key. Frequent deep-fried potatoes (fries) are linked with higher diabetes risk; baked or boiled potatoes do not show the same risk and can fit in a balanced plate—especially with the skin and alongside protein, veg, and healthy fats. (Harvard Chan School of Public Health)
Conclusion: Your Microbiome Is a Powerful Ally
The link between gut health and diabetes is strong—and scientists are learning more about it every year. A healthy gut can improve how your body uses insulin, reduce inflammation, and help keep blood sugar steady. Eating fiber-rich foods like beans, whole grains, fruits, and vegetables feeds good bacteria in your gut. Adding fermented foods such as yogurt, kefir, kimchi, or sauerkraut can boost beneficial microbes even more.
Choosing smart carbs—like brown rice instead of white rice—can prevent sharp glucose spikes. Pairing these habits with daily routines like staying active, drinking enough water, and getting good sleep can give your microbiome the steady support it needs. Small, consistent changes may seem simple, but over time they can lead to lasting improvements in both gut and blood sugar health.
Your turn: What’s one gut-friendly swap you’ll try this week—adding beans, a spoon of kimchi, or a new whole grain? Drop your choice (and any questions) in the comments!